
years.
11
We performed a single-arm phase II clinical trial of
PD0332991 in patients with progressive advanced WDLS/DDLS.
PATIENTS AND METHODS
To be eligible, patients had to be adults (age ⱖ18 years) with locally advanced or
metastatic WDLS/DDLS. In addition, patients had to have CDK4 amplification, as
detected by fluorescence in situ hybridization (FISH), and RB expression by im-
munohistochemistry, both determined on an archival tumor specimen.
Main inclusion criteria were histologically confirmed WDLS/DDLS, ad-
equate organ and marrow function, Eastern Oncology Cooperative Group
(ECOG) performance status of 0 or 1, and measurable disease by RECIST
(version 1.1).
12
Patients must have received at least one other systemic treat-
ment for advanced disease. All patients had evidence of clinical disease pro-
gression before enrolling onto this trial. The protocol was approved by the
institutional review board of Memorial Sloan-Kettering Cancer Center, and all
patients provided written informed consent.
Study Design and Statistical Analysis
This was a single-institution nonrandomized open-label phase II study.
The primary end point was progression-free survival (PFS) at 12 weeks. On the
basis of historical controls, PFS ⬎40% at 3 months was considered promising
for second-line therapy, and PFS ⬍20% was considered not promising.
13
A
one-stage design was used.
14
The initial study design called for a sample size of
28. The study would meet its primary end point if at least nine patients were
progression free at 12 weeks. This design has a type I error rate of 0.09 and a
type II error rate of 0.15.
CDK4 and RB Assessment
CDK4 amplification testing by FISH was performed using a probe com-
prising BAC clones RP11-571M6 (Wellcome Trust Sanger Institute, Hinxton,
United Kingdom) and RP11-970A5 (BACPAC Resources, Oakland, CA)
spanning CDK4, labeled with red deoxyuridine triphosphate, together with
chromosome 12 centromeric clone p
␣
12H8, labeled with green deoxyuridine
triphosphate (Enzo Life Sciences, Farmingdale, NY; supplied by Abbott Mo-
lecular, Chicago, IL).
FISH was performed on formalin-fixed, paraffin-embedded sections
according to standard procedures. Briefly, paraffin sections were dewaxed in
xylenes, microwaved in 10 mmol/L sodium citrate (pH, 6.0) solution for
approximately 10 minutes, cooled to room temperature, rinsed, and treated
with approximately 150 units/mL pepsin– hydrochloric acid for approxi-
mately 5 minutes at 37°C before being rinsed and dehydrated. Prewarmed
probe mixture was applied to the slides, and a coverslip was sealed in place with
rubber cement. The slides were then denatured at 80°C for 8 minutes on a
HYBrite automated hybridizer (Vysis, Des Plaines, IL) and incubated over-
night at 37°C. After standard nonformamide posthybridization washes, the
slides were stained with 4⬘,6-diamidino-2-phenylindole and mounted in anti-
fade (Vectashield; Vector Laboratories, Burlingame, CA).
Analysis was performed using a Zeiss Axioplan epifluorescence micro-
scope (Carl Zeiss Microscopy, Thornwood, NY) with motorized stage and Isis
5 imaging software (MetaSystems Group, Waltham, MA). Image records
consisted of collapsed stacks captured at 0.5-micron intervals through the
depth of the tissue. Amplification was defined as CDK4-to-centromere
ratio ⬎2.5, with a ratio ⬎10 representing high-level amplification.
RB expression by immunohistochemistry was determined using stan-
dard methods (RB [4H1] mouse monoclonal antibody; Cell Signaling Tech-
nology, Danvers, MA). Tumor samples were required to express RB at a
level ⱖ1⫹(above background).
Treatment
Patients were treated with 200 mg of PD0332991 once per day for 14 days,
followed by 7 days of rest. This was the maximum-tolerated dose determined in the
phase I study.
11
Cycles were repeated every 3 weeks, provided the following criteria
were met on the first day of the next cycle: platelet count ⱖ50,000/
L, absolute
neutrophil count ⱖ1000/
L, and hemoglobin ⱖ8.0 g/dL. If these criteria were
not met, the start of the cycle was delayed up to 7 days to allow for hematologic
recovery. If the start of the next cycle had to be delayed ⬎7 days, the dose was
reduced to 150 mg. In addition, the dose was reduced to 150 mg for grade 4
hematologic toxicity occurring at any time. If a second dose reduction was required
for the same reasons, the dose was reduced to 100 mg.
Response Assessment
Clinical examinations and laboratory testing were performed at a screening
visit, at the start of treatment, and at the start of each cycle of therapy for the first 12
cycles and thereafter at every other cycle. In addition, a complete blood count was
performed once per week during the first cycle. Tumor response was assessed by a
reference radiologist by computed tomography (CT) scan once every 6 weeks
(regardless of dose delays) for 36 weeks and once every 12 weeks thereafter. Toxic-
ities were assessed and graded according to the National Cancer Institute Com-
mon Terminology Criteria for Adverse Events (version 4.0).
RESULTS
Between October 2010 and November 2011, 51 patients gave consent
to the protocol. The flow of patients and tumor testing is described
Consent obtained
(n = 51)
Tested for CDK4
(n = 48)
Tested for RB
(n = 44)
CDK4 amplified and RB expressed
(n = 41)
Treated on study
(n = 30)
Analyzed for the primary end point
(n = 29)
Patients excluded (n = 3)
)1 = n( sedils oN
Ineligible (n = 2; patients with disease
other than WD/DD LPS)
No CDK4 amplification detected
(n = 4)
RB not detected (n = 3)
)1 = n( eruliaf tseT
Test not completed (n = 2)
Patients not treated (n = 11)
No prior systemic therapy (n = 6)
No disease progression (n = 2)
)3 = n( eciohc tneitaP
Excluded from analysis of (n = 1)
primary end point
Withdrew consent before (n = 1)
completing one cycle of
treatment
Fig 1. Diagram showing flow of patients and testing for CDK4 and retinoblastoma
protein (RB). DD, dedifferentiated; LPS, liposarcoma; WD, well differentiated.
Phase II Trial of the CDK4 Inhibitor PD0332991 for Liposarcoma
www.jco.org © 2013 by American Society of Clinical Oncology 2025
from 128.122.114.215
Information downloaded from jco.ascopubs.org and provided by at NEW YORK UNIVERSITY MED CTR on July 22, 2013
Copyright © 2013 American Society of Clinical Oncology. All rights reserved.
 2024-11-15 27
2024-11-15 27
 2024-11-15 16
2024-11-15 16
 2025-04-07 11
2025-04-07 11
 2025-04-07 7
2025-04-07 7
 2025-04-07 11
2025-04-07 11
 2025-04-07 7
2025-04-07 7
 2025-04-07 8
2025-04-07 8
 2025-04-07 6
2025-04-07 6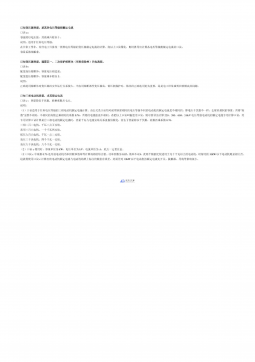
 2025-04-07 8
2025-04-07 8
 2025-04-07 11
2025-04-07 11







 渝公网安备50010702506394
渝公网安备50010702506394
